Hypovolemic shock is a very serious condition that can put lives at risk. It happens when your body doesn’t have enough blood or fluids. Recognizing the symptoms early can save lives, making awareness super important. This article will guide you through what hypovolemic shock is, its causes, warning signs, stages, and how it’s treated.
Demystifying Hypovolemic Shock: What is it?
Hypovolemic shock comes from the body losing a lot of blood or fluids quickly. This makes it harder for your heart to pump enough blood to your body. What makes it so dangerous is its swift progression compared to other types of shock. It can lead to vital organs failing if not treated right away.
Some people confuse it with other medical issues, but it’s unique. Unlike other shocks where the heart might stop working properly, hypovolemic shock directly relates to the volume of blood loss.
Misunderstandings about hypovolemic shock usually arise from its symptoms, which can mimic other illnesses. However, understanding its true nature helps in early detection and treatment.
Body’s Battle: How The Body Reacts to Low Blood Volume
When blood volume drops, your body goes into action mode. Your heart starts beating faster, and your blood vessels tighten up. This is the body’s attempt to keep blood moving to your vital organs. But, the longer this lasts without treatment, the more dangerous it becomes.
If hypovolemic shock is not managed quickly, it can lead to organ failure. Getting medical help fast is crucial. Every minute matters in treating this condition.
Root Causes of Hypovolemic Shock
Hypovolemic shock can occur due to several reasons. The main cause is external bleeding, like from a car accident or a severe cut. Internal bleeding from organs, such as a broken bone, can also cause it.
- Severe burns or severe diarrhea can lead to massive fluid loss,
- Heatstroke and heat exhaustion often lead to dehydration, contributing to the condition.
Common injuries, illnesses, and even some surgeries can trigger hypovolemic shock. That’s why it’s critical to monitor fluid levels and heed any warning signs.
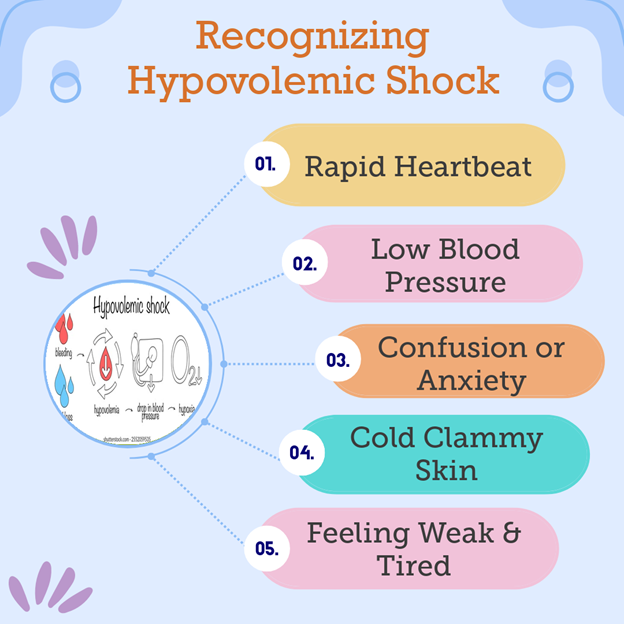
Spotting the Signals: Symptoms of Hypovolemic Shock
Symptoms of hypovolemic shock can vary. In adults, signs include confusion, cold skin, and rapid breathing. For kids, there might be irritability and reduced alertness.
Age and health status impact how symptoms show. Pediatric symptoms differ because kids’ bodies respond differently to blood loss.
Early recognition is vital. Quick response can save lives, so it’s important to react when these symptoms appear.
From Bad to Worse: Understanding Stages of Hypovolemic Shock
Hypovolemic shock progresses through four stages. Each stage gets more serious and has specific signs:
- Initial Stage: Slight increase in heart rate.
- Compensatory Stage: Rising heart rate, cool skin, sweating.
- Progressive Stage: Rapid breathing, confusion.
- Refractory Stage: Organ failure risk.
The quicker you catch it and get help, the better! Action during early stages is crucial to managing progression.
Consequences of Ignoring Hypovolemic Shock
Ignoring hypovolemic shock can be deadly. It can cause organs to stop working. If ignored, the damage could be permanent.
People can suffer long-term health effects if untreated. Fast medical help is the only way to stop permanent damage. Immediate action prevents tragic outcomes.
Diagnosing Hypovolemic Shock: What to Expect
Doctors use several steps to diagnose hypovolemic shock. They’ll check physical symptoms like cool skin and rapid breathing.
Technology plays a big role. Devices measure heart rate and blood pressure quickly.
The quicker the assessment, the better the outcomes. Rapid diagnosis saves time and lives.
Life-saving Measures: Hypovolemic Shock Treatment Options
When hypovolemic shock is suspected, immediate action is key. Lie the person down and raise their legs if possible. This can help improve blood circulation.
In hospitals, the first step is usually to give IV fluids. This helps raise the blood volume quickly.
If the shock is due to blood loss, blood transfusions might be necessary. They restore lost volume and help stabilize the patient.
Sometimes, surgery is needed to fix issues causing the blood loss. Your doctor might also prescribe medication to help improve blood pressure and heart function.
These treatments work together to treat hypovolemic shock effectively, ensuring the best chances for recovery.
The Journey Back: Recovery and Long-term Outlook
Recovery from hypovolemic shock varies. Factors like how fast treatment was and overall health play a big role.
Some people experience long-term health effects and might need rehabilitation.
Ongoing medical care is important to monitor and manage any lasting symptoms, ensuring a good quality of life.
Staying Ahead: Preventing Hypovolemic Shock
Prevention is the best approach. Avoid injuries by wearing protective gear during risky activities.
Stay hydrated, especially during hot weather or exercise.
Manage health conditions that could lead to fluid loss. Seek medical care early if bleeding or severe dehydration occurs, reducing the risk of shock.
Conclusion
Hypovolemic shock is dangerous but knowing the signs can save lives. Be aware and ready to act fast.
Learning basic first aid and recognizing symptoms is crucial. Understanding preparedness can make a big difference.
Stay informed and stay safe.
In case of emergency, trust Sun Hospitals—your partner in critical care and life-saving response. Be prepared. Act fast. Save lives.

